What is keratoconus?
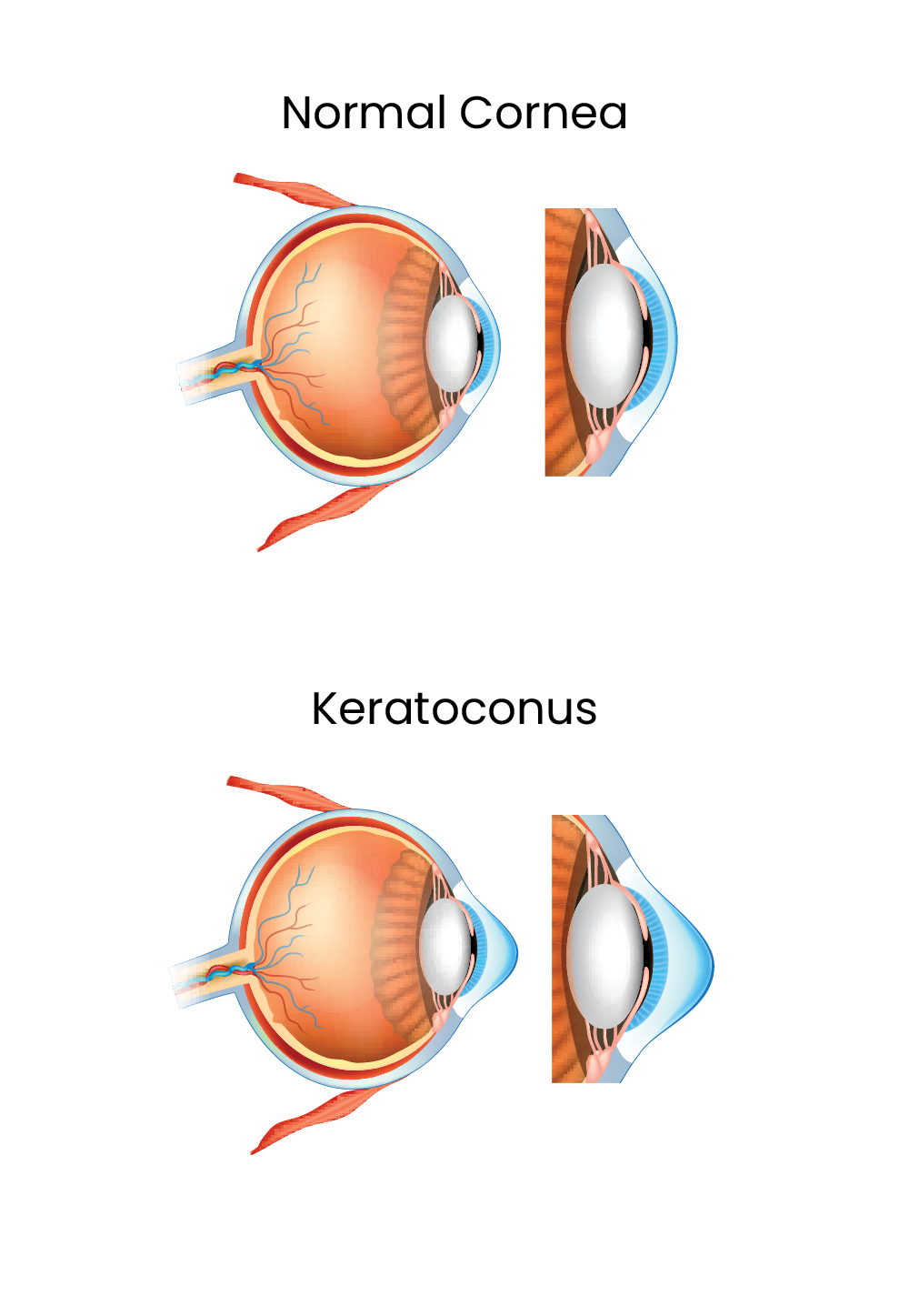
Keratoconus is a condition that causes thinning and bulging of the cornea, the front surface of the eye that allows light to enter.
It is a progressive condition that distorts the cornea’s shape. While
the condition is present from birth, most people do not experience symptoms until they are between the ages of 10 and 25 years
What are the symptoms of keratoconus?
- Blurred or distorted vision
- Cloudy vision
- Light sensitivity
The distorted cornea shape results in blurred or reduced vision and increased eye sensitivity.
What causes keratoconus?
The exact cause is uncertain, but a genetic link seems likely, as the incidence rate is greater if a family member has been diagnosed. Keratoconus disease affects approximately one person in every 1000. Experiencing seasonal allergies and asthma can be additional risk factors, and the associated rubbing of the eye can make the condition worse.
How we diagnose keratoconus
Diagnosis
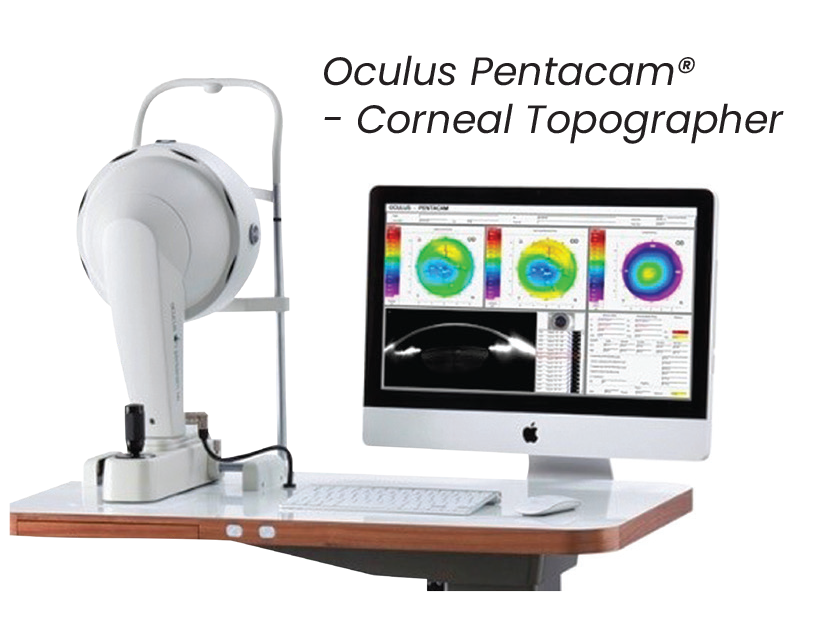
There are a range of vision and corneal measurement assessments we can use to diagnose and monitor your keratoconus symptoms.
Refraction testing checks for problems in vision, and uses combinations of different lenses to improve your eyesight. This is the basis for for vision correction corrective glasses.
Corneal topography records the shape of the eye’s surface and is used to monitor your condition’s progression – how your eye is changing – over time.
Once keratoconus progresses, corneal thickness testing (pachymetry) is another simple and painless way of tracking corneal measurements.
Other Ectasia
- Terrien’s Marginal Degeneration
Terrien’s Marginal Degeneration is a progressive and degenerative thinning of the cornea, usually in the superior (upper) margin of the cornea. It is more commonly seen in males over the age of 40. As the condition progresses, the corneal thinning can extend the entire circumference of the cornea. It can be inflammatory in nature, with neovascularisation (blood vessel growth), lipid deposits and corneal scarring commonly seen.
- Pellucid Marginal Degeneration
Pellucid Marginal Degeneration is a progressive, degenerative, noninflammatory corneal condition. It is commonly confused with Keratoconus as it also results in thinning of the cornea, however the area of thinning is typically localised to the inferior (lower) and peripheral cornea. Like Keratoconus, patients often present with irregular astigmatism, and vision that can no longer be adequately corrected in glasses or contact lenses.
- Keratoconus Diagnosis
Keratoconus is diagnosed with a comprehensive eye exam and a discussion of your history of keratoconus disease symptoms. We will carefully analyze the surface and characteristics of your cornea using advanced diagnostic technology. We will also take precise measurements of your cornea to get a baseline idea of its shape, and continue to take annual measurements to detect and track changes.
How we help treat keratoconus
Everyone’s experience of keratoconus is different and the best treatment at one stage will be different to that at another stage. Our highly experienced eye health professionals can provide advice and guidance to suit your needs.
Keratoconus glasses
Glasses can help your vision in the early stages of keratoconus. Over time however, with the progression of your condition, you may require frequent changes.
Contact lenses
In many cases, people experiencing keratoconus will require rigid contact lenses to improve their vision. These lenses are better able to correct the cornea’s irregular shape.
Corneal collagen cross-linking
This advanced keratoconus treatment can stabilise vision and delay the progression of keratoconus. It uses vitamin B2 and ultraviolet light exposure to strengthen the corneal collagen fibre connections. This can help to stabilise the cornea.
Corneal Transplant
Up to one in four people who experience keratoconus may require a corneal transplant. This operation removes the distorted tissue and replaces it with healthy donor tissue.
Frequently Asked Questions
Can I have LASIK if I have keratoconus?
No, keratoconus is a contraindication for LASIK. There is a risk that removing corneal tissue during LASIK or other forms of laser eye surgery may make an already-degenerating cornea more unstable.
Can keratoconus cause blindness?
Keratoconus normally does not cause complete blindness. However, if left untreated, vision can significantly deteriorate to the point that it becomes difficult to read, drive or perform other daily tasks.
Can keratoconus cause dry eye?
Keratoconus may lead to dry eye symptoms. When the cornea is irregularly shaped, the tear film may not be able to spread evenly over the ocular surface, and the eyes can become dry, itchy or irritated. Wearing contact lenses for keratoconus can also increase the likelihood of developing dry eye symptoms.
If one of my parents has keratoconus, am I at a higher risk?
Doctors are still learning about why keratoconus develops and the factors that make someone more likely to get the disease.
It seems that keratoconus may run in some families. If one of your parents or siblings has keratoconus, you are at a greater risk of getting it.
Also, if you have atopy or chronic hay fever or eczema, you are at an increased risk of developing keratoconus.
What will my vision look like if I get keratoconus?
The abnormal shape of the cornea can lead to significantly distorted vision (similar to what you would see if you looked in a carnival funhouse mirror). You may develop nearsightedness or see double or triple “ghost” images, glare or streaks when looking at bright lights.
In most cases of keratoconus, both eyes are affected — however, each eye may be affected in different ways.
Can keratoconus make it hard to see when driving at night?
Yes. The effects of keratoconus can cause you to see starbursts, glare or halos around bright lights. At night, these visual aberrations may make it nearly impossible to see your dashboard, the road, road signs and oncoming headlights.
Will keratoconus go away on its own?
No. Although the severity of the disease varies by patient, keratoconus is a chronic, degenerative condition that will not improve without treatment.
If you have recently been diagnosed with keratoconus, our doctors encourage you to promptly schedule a consultation to discuss your treatment options.
How is corneal crosslinking performed?
Corneal crosslinking is an outpatient procedure that takes about one hour to complete. First, riboflavin (vitamin B12) drops are administered to the eyes. Then, the eyes are exposed to ultraviolet light. This creates a chemical reaction that strengthens the collagen fibers in the cornea, thereby improving the cornea’s stability.
The procedure has a high success rate. Undergoing corneal crosslinking can stop the progression of vision loss to keratoconus and prevent the need for more invasive treatment (e.g., corneal transplant surgery).
If glasses no longer provide suitable vision correction after corneal crosslinking, our team can explore other options, such as implantable contact lenses or specialty contact lenses.
Do you have a question or concern about your eye health? To discuss your condition with an experienced ophthalmologist or optometrist, please contact The Eye Health Centre


